Free download: Top 10 Natural & Easy Remedies for Joint Pain from Home. Learn these helpful remedies.
Estimated Reading Time: 11 minutes read
You have this nagging pain on the bottom of the heel that just won’t go away… It started off barely noticeable, but now it feels worse. It’s been weeks… Maybe months…
What’s happening here??
There are many possibilities as to what could be causing your heel pain. The Royal College of Surgeons of England states that “7% of people over 65 years of age report tenderness in the heel.”
Two of the most common causes of heel pain include heels spurs and plantar fasciitis. If they both cause heel pain though, how can you tell the difference? Is it a heel spur or plantar fasciitis causing the pain?
Here’s a more important question: How can you make this foot pain go away?
A detailed comparison of both heel spurs and plantar fasciitis should help to clarify the differences between the two and what can be done to treat them.
Table of Contents
Heel Spurs
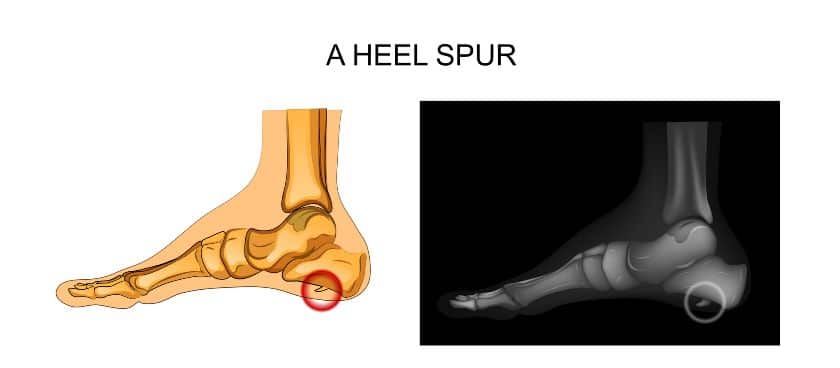
Heel spurs are bone spurs that involve bony growths on the heel bone.
While the exact cause is not clearly understood, it’s thought that heel spurs happen when there is repetitive stress to the heel bone, such as with running and jumping, can create abnormal calcium deposit growth.
Heel Spur Symptoms:
The following are common symptoms of heel spurs:
- Dull ache in the heel
- Gait abnormalities
- Heel spurs can also feel like a sharp pain that worsens with increased activity
- Pain is relieved with rest and/or stretching
Treatment of Heel Spurs:
There are various conservative methods for treating a heel spur. This may include one or more of the following:
- Rest
- Stretching/foot and ankle exercises
- Physical therapy
- Steroid injections, such as cortisone injections, to reduce inflammation and pain
- Anti inflammatory medications
- Orthotics inserts, such as a heel cup or heel pad, in supportive shoes to cushion the painful area
- Well fitting shoes
It’s not very common, but in some cases if conservative treatments fail, heel spur surgery may be necessary to remove the heel spur. The challenge with this is not being able to know definitively if removing the heel spur will fully relieve pain, as there can be mixed results among individuals who undergo surgery.
Plantar Fasciitis
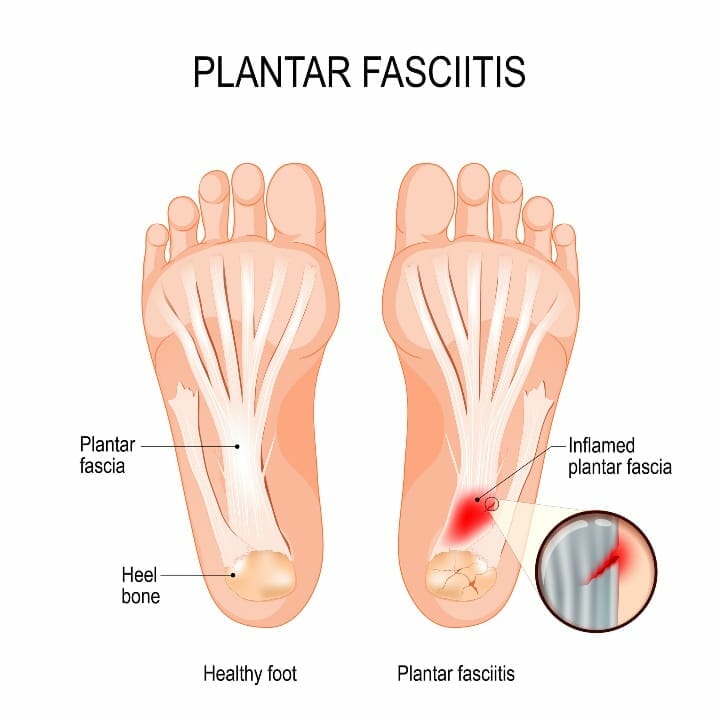
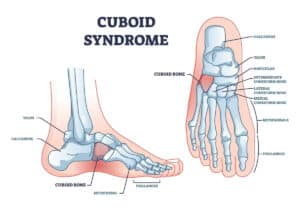
Plantar fasciitis pain occurs on the bottom of the foot, where the plantar fascia runs. It’s a thick band of connective, soft tissue that plays a large role in supporting and stabilizing the foot arch.
Plantar fasciitis is typically caused from excessive stress or trauma in the area where the plantar fascia begins at the heel. This can lead to an inflammatory response and a subsequent painful foot.
Plantar Fasciitis Symptoms:
If you’re experiencing plantar fasciitis, you may notice one or more of the following symptoms:
- Arch or heel pain with passive stretching of the toes back into extension
- Arch or heel pain worse in the mornings
- Arch or heel pain worse when standing after having rested for a while
- Pain may improve initially with walking, but worsens with extended walking or exercise
Treatment for Plantar Fasciitis:
Conservative treatment of plantar fasciitis may include one or more of the following:
- Nonsteroidal anti inflammatory medication
- Steroid injections, such as cortisone injections, to reduce pain and inflammation
- Stretching exercises for the plantar fascia and Achilles tendon
- Foot/ankle strengthening exercises
- Orthotic devices (e.g., shoe inserts for the heels, heel pads, night splints)
- Well fitting shoes
Similar to a heel spur, if conservative measures fail, a plantar fascia release may be necessary. This is where the plantar fascia ligament is surgically released to relieve pain.
Plantar Fasciitis AND a Heel Spur
Curveball here…
There are instances when you can have BOTH plantar fasciitis and a heel spur. It’s thought that the inflammation that typically accompanies plantar fasciitis can lead to the creation of the calcium deposits in the heel, causing development of a heel spur.
While plantar fasciitis doesn’t always involve the presence of a heel spur, it can be more common to find a heel spur accompanied by plantar fasciitis.
Confirming a Diagnosis
As you can see, there are quite a few similarities in the symptoms and management of heel spurs and plantar fasciitis.
So, how do you differentially diagnose between the two when you have heel pain?
Physical Examination:
A medical doctor or physical therapist can perform an in-person physical exam to determine what exactly is going on.
This will normally involve taking a thorough past medical history, which can reveal if you have predisposing risk factors placing you at a higher risk for either diagnosis, as well as testing range of motion, strength, finding areas of tenderness, and assessing your functional limitations from the heel pain.
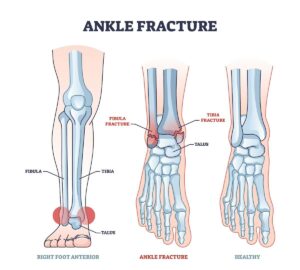
Sometimes additional imaging may be necessary to confirm the presence of a heel spur. This may involve an X-ray or MRI.
Risk Factors:
There may be some factors in your medical history that reveal an increased chance of developing plantar fasciitis and bone spurs.
Take a look at the following possibilities:
- Arthritis in the foot or ankle
- Poor shoe wear
- Obesity
- Decrease ankle flexibility, especially with ankle dorsiflexion
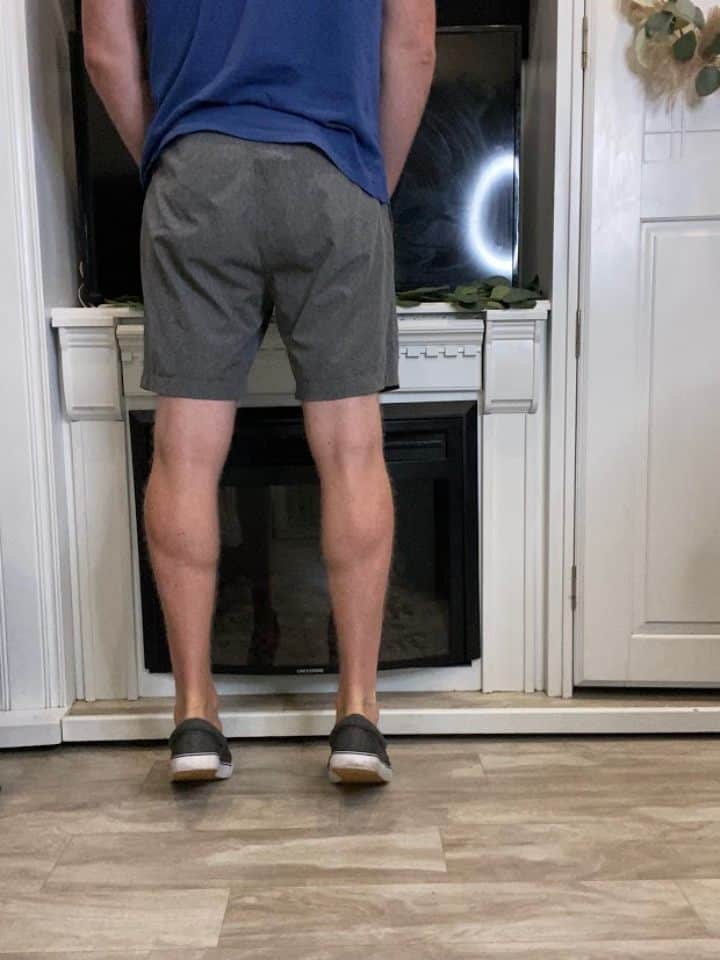
- Tight muscles, especially in the calves
- High arches
- Flat feet
Recommended Exercises for Heel Pain
Exercise is included as a recommended measure to address heel pain, regardless of if the heel bone pain is caused by heel spurs or the plantar fascia.
Let’s look at a few simple plantar fascia and heel spur exercises that involve stretching and strengthening. You’ll likely encounter these if you’re going through physical therapy to address your heel pain.
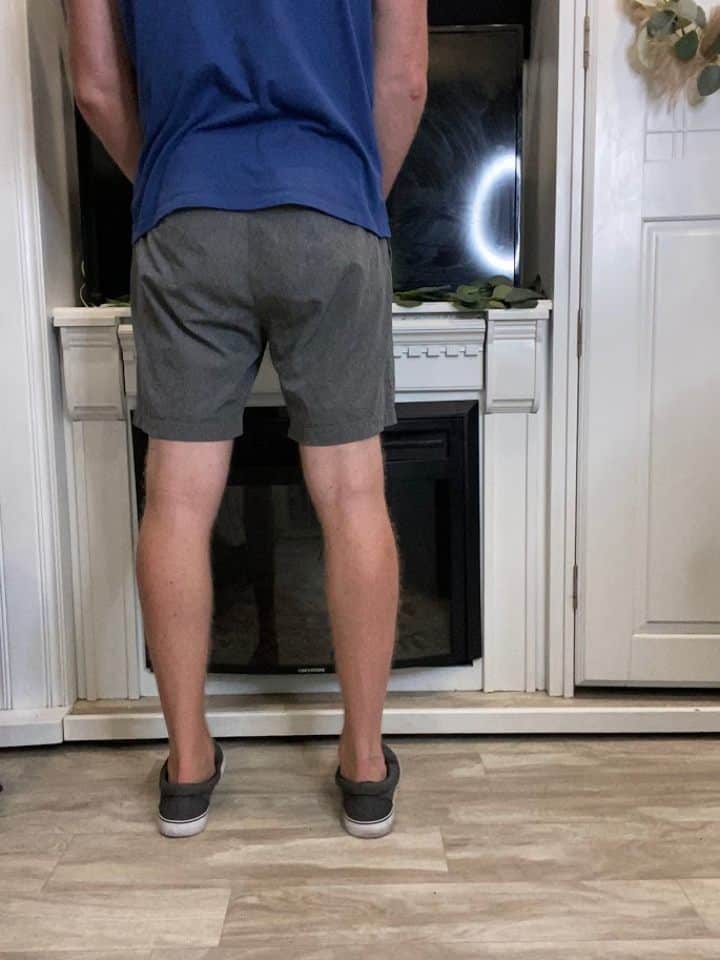
Standing Calf Stretch:
Due to having a higher risk of developing heel spurs and plantar fascia pain from tight calves, it’s important to make sure you’re including calf stretches into your daily routine.
There are two primary calf muscles addressed with a standing calf stretch, gastrocnemius and soleus. For each muscle to be properly stretched, this will require a little variation in the exercise between the two.
Gastrocnemius calf stretch:


- You can begin by standing facing a wall or other supportive surface with the feet together.
- Take one step forward with the non-painful leg and keep the affected foot behind.
- Bend the front knee slightly and keep the back knee straight.
- As you feel a stretch in the back calf, hold at least 30 seconds or up to 1 minute.
- You can switch legs to keep things symmetrical.
Soleus Calf stretch:


- Move into the same starting lunge position as the gastrocnemius calf stretch.
- This time, slightly bend both the front and back knees.
- As you feel a stretch in the back calf, and probably more of a pull in the heel, hold at least 30 seconds or up to 1 minute.
- Switch legs.
*Tip: Make sure both heels remain flat on the floor during the stretch. If you’re looking for a stronger stretch, you can move the legs further apart into a deeper lunge.
Standing Calf Raises
Standing calf raises are a simple way to strengthen the calf muscles. If the calf muscles are more on the weak side, this can create abnormal forces at the foot and ankle, including the heel, increasing your chances of heel bone pain.
- Stand facing a wall or other sturdy surface if you need help to balance.
- Place the feet side by side, about hip width apart.
- Slowly lift the heels from the floor as high as you can, then lower back down.
- Repeat 10-15 repetitions for 2-3 sets.
Advance your calf raises:
You can easily increase the challenge of your calf raise by practicing higher repetitions or by performing on one leg at a time.
To perform the calf raise on one leg at a time, do the following:

- Position yourself just like the double leg calf raise, only now stand on one leg.
- Slowly raise the heel from the floor as high as you can (without straining), then lower back down.
- Repeat 5-10 repetitions to begin with for 2-3 sets.
*Tip: As a single leg calf raise is considerably more challenging, don’t try to force the range or number of repetitions. Begin with a smaller range of movement and fewer repetitions initially, then you can advance the movement and repetitions as able.
Step Stretch
If you have access to a step (anywhere from 4-8 inches in height), this is a great tool for stretching the areas around the foot and ankle.


- Facing a single step around the above-mentioned height, place the affected side forward on the step. The other leg will remain on the floor.
- Lean forward towards the front leg, keeping the heel down, until you feel a stretch in the area of the heel, Achilles tendon and/or calf.
- Hold the stretch for at least 30 seconds or up to 1 minute.
- Switch legs for a symmetrical stretch.
How to Use a Step for a Great Leg Stretch
Shoe Wear to Consider
A recommendation for heel spur pain and/or plantar fascia pain is to check that you’re using the proper shoe wear.
Make sure to wear appropriate shoes that fit you well. For our ladies out there, try to avoid wearing heels if you’re having heel pain, as this tends to position the foot and ankle into a plantarflexed position, which shortens the calf muscles.
This can contribute to further calf tightness.
You may need to consider adding in an over the counter shoe insert or heel cup to cushion and support the arch and heel. If an over the counter option is not successful to reduce pain, you may need custom made orthotics.
How Sleeping Position Can Contribute to Pain
You may not normally consider your sleeping position as a contributing factor for heel spur pain or plantar fascia pain, but it actually is very relevant.
Normally when we sleep, the feet and ankles tend to end up in a plantarflexed position, which if you recall, places the calf muscles in a shortened position.
If you lay like this all night, when you first get up in the morning you’ll notice greater pain, especially with plantar fasciitis. The reason is because when you take a step, you have to dorsiflex the ankle for your heel to strike the ground to initiate a step.
This is the complete opposite position you just slept in all night, so tightness in these soft tissues can create pain.
Simple Treatment Methods
When you first begin experiencing heel pain, try to begin starting simple treatment methods as soon as possible. This will help reduce your pain and avoid development of chronic pain.
If you’ve tried the recommended treatments on your own at home, and are still having pain, consider seeing a professional healthcare provider for a more in-depth assessment and additional recommendations.
It will be worth it to get rid of that nagging heel pain!
FAQ:
How long does a heel spur last?
Unfortunately, a heel spur typically doesn’t go away. Just because you have a heel spur though, doesn’t mean you will always have pain. There are many people with heel spurs who don’t have associated pain.
If, however, you have intense pain associated with a heel spur and have failed conservative efforts, surgery to remove may be recommended. It’s important to note though that surgery can’t guarantee complete resolution of your pain.
How long is the recovery time for heel spur surgery?
This answer will vary from person to person. Generally speaking, you can expect at least a few weeks before you’re walking more normally again. Initially you may be given weight bearing restrictions to allow full healing.
While it will definitely take at least a few weeks to recover, some may heal more slowly and may require a few months for recovery.
Is there a certain age you’re more likely to develop a heel spur?
Not necessarily. It all depends on the true cause of the heel spur.
If the cause is related to arthritis, then normally those who are older, such as 50+, will experience this. If the cause is related to activity, shoe wear, repetitive stress or development of plantar fasciitis, then really anyone at any age could develop this.